How cellular software can help us to decode cancer
Co-Head of the Women’s Cancer Program
- What happens with cancer is that the cell’s code is corrupted. As cancer researchers, we try to understand how that code is corrupted in each patient.
- Ovarian cancer is not one disease: it’s actually many distinct diseases that share an anatomical location in the body.
- The real achievement in the last decade has been the development of fast, affordable instrumentation that can sequence the DNA of patients’ cancers.
What is a genome?
We’re all familiar with computers and how they have an embedded operating system, which could be Windows, Mac, or something more exotic; but, in fact, the first embedded operating systems were invented close to four billion years ago. It’s what we call the genome: the code that allows cells to divide, multiply and specialise. In the case of the computer, the operating system is made out of silicon; in the case of the genome, it’s made out of long strands of DNA. Somewhat like a hard disk, the DNA is packaged up in an organelle – the nucleus, the centre of the cell – and that’s the repository of information that a cell relies on to divide and propagate.
What happens with cancer is that the code is corrupted in different ways. It could be corrupted by walking out in the sunshine and the UV light damaging the DNA and changing the code subtly, to then start the process of cancer. So, what we do as cancer researchers is we try to debug the code to understand how that code is corrupted in each patient and how that will affect the growth of their cancer and the response of the cancer drugs.
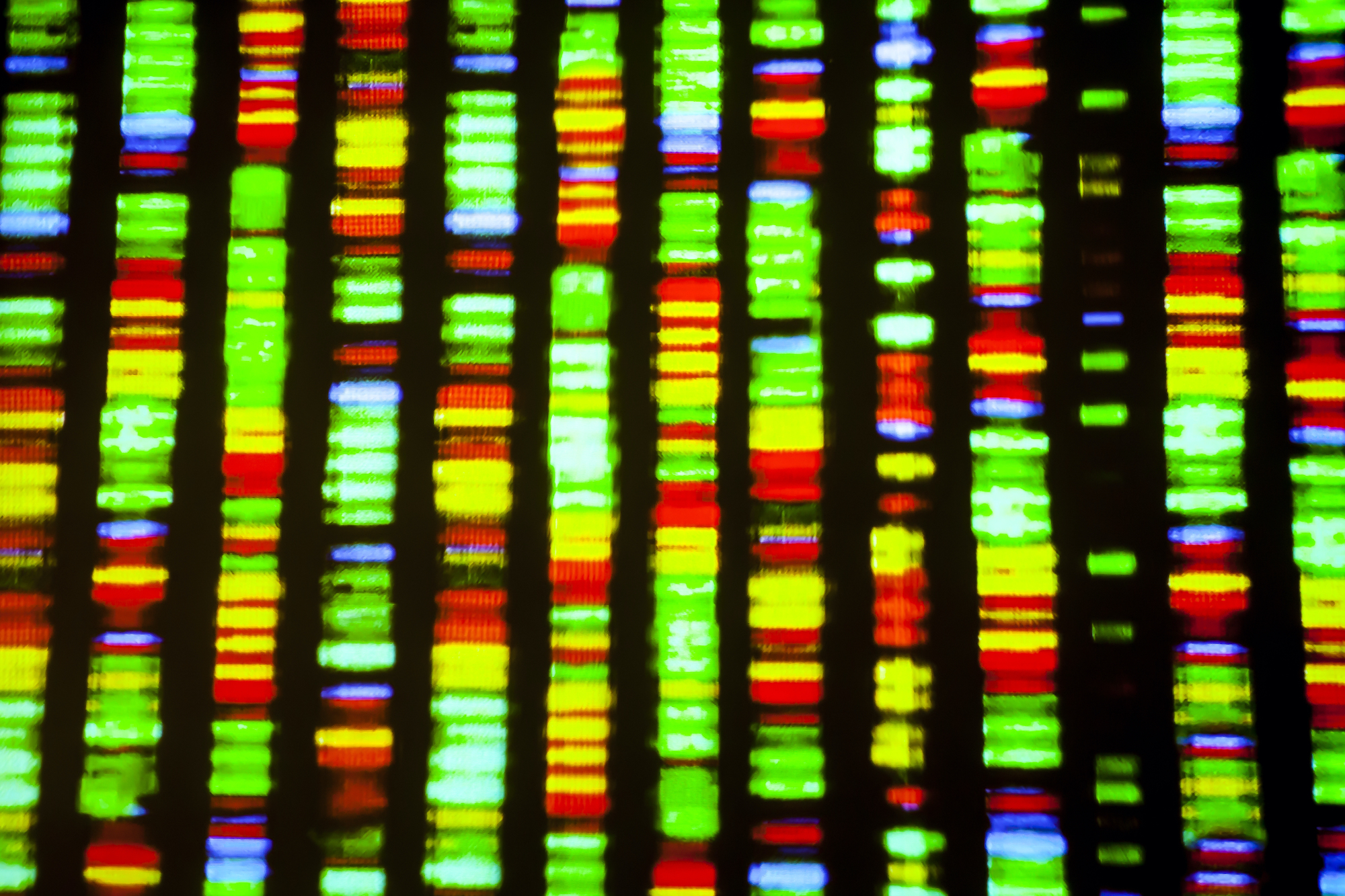
DNA sequence. By Gio.tto.
Understanding the error
To follow the analogy of software and cells, what we need to be able to do in a patient to determine the cause of cancer is to understand the nature of the error in that particular patient. We do that by sequencing the DNA from the cancer cells. This is now actually a routine part of clinical practice in cancer centres the world over: to assess the software errors and to match those errors with drugs that can treat the particular problems in the cancer cells.
Many of these errors involve genes that make enzymes. These are proteins that catalyse chemical reactions and drive the cancer cells towards division, multiplication, and the formation of a mass that we’re familiar with as cancer. So, the new drugs that have been developed target these enzymes and shut them down, and that’s one way that we can personalise cancer therapy.
Similarities between cancers
One of the by-products of getting inside the code of cancer cells is that we now find similarities between cancers that are in quite different parts of the body. For millennia, we have thought about cancers from an anatomical perspective – someone has breast cancer, or prostate cancer, or kidney cancer. But once we started to read the code in the cancers, we found that the cancers needed to be reclassified. The cancers that were quite widely spaced in the body, for example ovary and breast cancer, turn out to have molecular similarities – similarities in this software code – in the way that the code is disrupted.
The most common type of ovarian cancer, called high-grade serous ovarian cancer, is actually very closely related to a particularly aggressive type of breast cancer called triple-negative breast cancer. Those two belong together in terms of their classification, because they behave similarly, from a genetic point of view. They respond to treatments in a similar way and they have a similar type of growth profile.
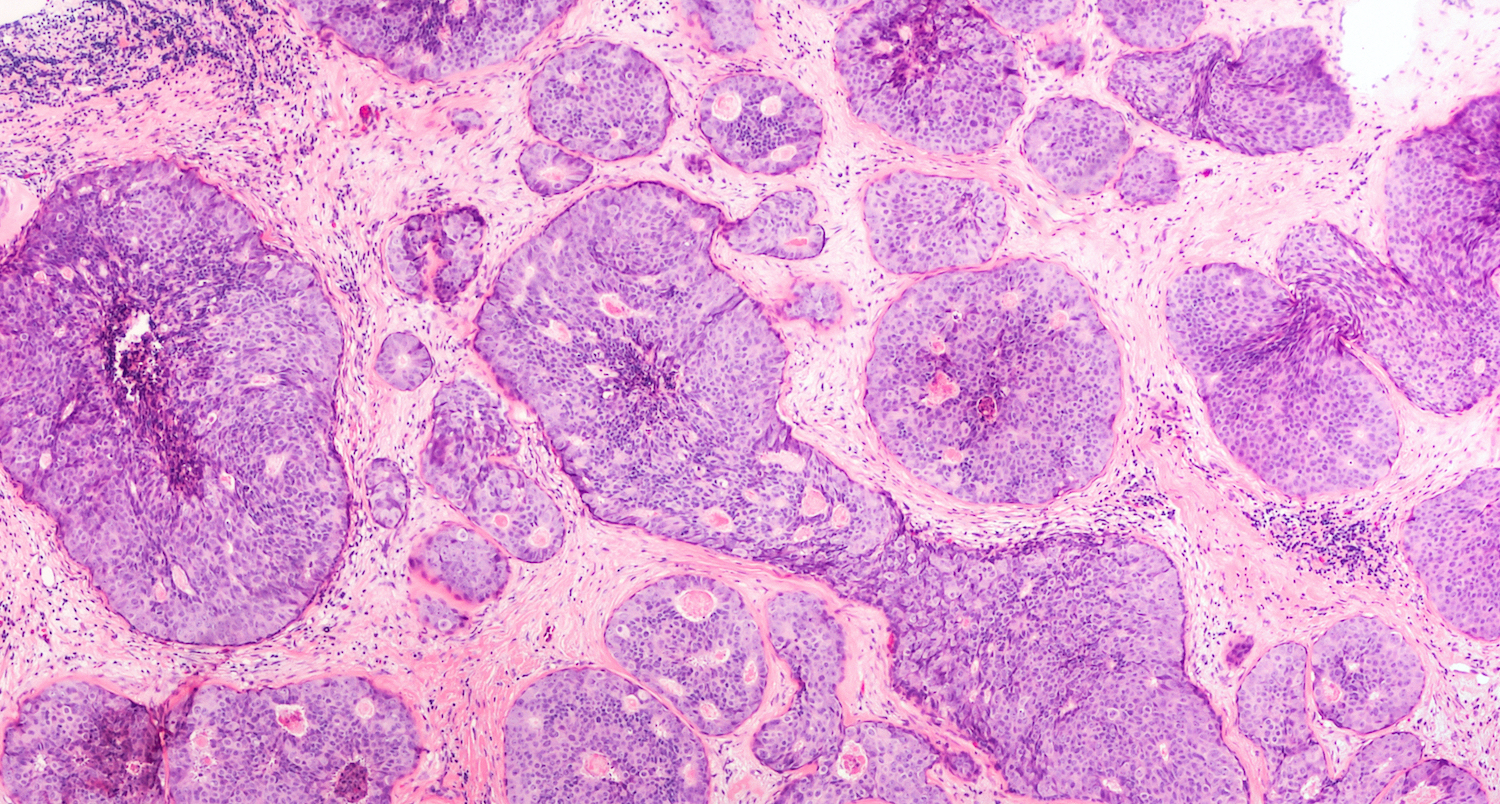
Breast cancer core biopsy. By David A Litman.
Cancer is not a single disease
Now that we have started to reclassify cancers based on their software – on their molecular biology – we can see that what we once regarded as a single cancer, or maybe just a few cancers, is actually very distinct. If you take ovarian cancer as an example, we find that it’s certainly not one disease: it’s actually many distinct diseases that share an anatomical location in the body, but are very different in terms of the drugs that they respond to and the way that they behave in terms of their growth. What we also find, surprisingly, is that most of the ovarian cancers that actually kill women are not from the ovary. They are from cells that surround the ovary. Different versions of ovarian cancer come from different types of cells, and then they tend to lodge in the ovary and grow there. It might seem to be a fine point, but it actually influences the way that we can manage genetic risk in women with ovarian cancer, and also understand that these cancers have to be treated as distinct entities. A one-size-fits-all approach does not work when you’re treating ovarian cancer.
Ovarian cancer subtypes
To continue with ovarian cancer, an analogy may be helpful. We all know about Russian dolls, the Babushka dolls, where you think that something’s just a single entity, but when you open the lid, you find that there’s a doll within the doll, and then you open it again and you find that there’s another doll within the doll. The same thing has happened in the case of ovarian cancer. We thought of it as one disease, but as we have picked apart its biology, we have found that there are many subtypes. The most common type of ovarian cancer is high-grade serous ovarian cancer. Initially, it splits into two groups: one group that has a particular defect in the way that it repairs DNA and another group where that process is intact. Within the group where it’s intact, there’s another group that requires a distinct type of treatment, and that’s part of a clinical trial that we’re working on at the moment. The group that has this defect in DNA repair tends to benefit from a new class of drugs called PARP inhibitors, which have been very successful in treating that particular subtype.
Understanding cancer cells
Understanding the software code in cells seems easy, but it’s actually very hard. To give you a sense of scale, if we isolated some tissue from a person or an animal and we pulled out all the nuclei that have this DNA code in them, and we smush them into a little cube, this one centimetre by one centimetre by one centimetre would contain enough DNA to stretch 12 million kilometres. It contains about 10,000 petabytes of data. So, again, to put that into computing perspective, that’s the equivalent of the storage of about a thousand fridge-sized racks of computer storage. That’s just from one centimetre of nuclei – we have, roughly, a trillion cells in our body, so the complexity of the code is enormous. And that’s just the normal code. When you come to a cancer cell, that code has been shuffled and has bugs in it. We need to understand how those errors in the code translate into the behaviour of cells in cancer. That’s what makes cancer such a complicated problem.
Exceptional survivors
One of the groups that we’re fascinated by is the exceptional survivors: women who have beaten the odds. This is an emerging area of cancer research, and it’s not just applicable to ovarian cancer: it’s true of any cancer group. There will be patients who, despite all expectations, are still alive 10 or 15 years later, sometimes completely free of their disease. Sometimes they’ve lived with this crumbling disease over that time. This is a concept that can be carried forward, in the study of these patients, to a whole variety of cancer groups. In fact, it probably even applies outside of cancer.
We recently wrote a perspective on how you study these exceptional survivors. I was contacted by a researcher from James Cook University in northern Queensland who is studying exceptional survival in corals that are affected by climate change and coral bleaching. So, the same concepts of survival against the odds could be used in studying the dynamics of survival in all sorts of environments.
Therapies for drug resistance
Because ovarian cancer has been reclassified by the basis of its software, it turns out that there are similarities that are not expected from an anatomical perspective. High-grade serous cancer is very similar to triple-negative breast cancer. Our lab is part of a programme funded by the US National Institutes of Health to study the systems biology of breast and ovarian cancer and the emergence of drug resistance in patients with those cancers. What we’ve found is that one of the mechanisms of resistance to drugs that occurs in ovarian cancer also occurs in breast cancer and in prostate cancer. So, once you identify that, it suggests therapeutic approaches that can be used not just in one disease, but in the other diseases.

Antibiotic resistance concept. By The26January.
An important achievement
Cancer, as a cellular software problem, is complex but, ultimately, understandable. We now have really sharp tools to decipher the code. For decades, we have been on the outside looking in. Again, to use a laptop analogy, imagine that you are trying to understand a laptop by staring at the screen. You would never understand that there was a code operating there of ones and zeros and how that software code was controlling PowerPoint or Windows. The same is true about cells. For hundreds of years, we’ve just looked from the outside – initially, at a mass, then, as microscopes were developed, at cells. But really, until we could get at the code itself, by sequencing DNA, we could never really understand what was occurring. The real achievement in the last decade has been the development of fast, affordable instrumentation that could read the software code, that could sequence the DNA of patients’ cancers, and allow us to interpret what occurred in their cancer, what was driving it and how it might respond to drugs.
Discover more about
cancer research
Cheasley, D., Nigam, A., Zethhoven, M., et al. (2021). Genomic analysis of low-grade serous ovarian carcinoma to identify key drivers and therapeutic vulnerabilities. Journal of Pathology, 253, 41–54.
Freimund, A. E., Beach, J. A., Christie, E. L., et al. (2018). Mechanisms of Drug Resistance in High-Grade Serous Ovarian Cancer. Hematology/Oncology Clinics of North America, 32(6), 983–996.