Obviously, we want our politicians to resolve these challenges. But what can innovation and science really do for something as complicated as public health, as well as for infectious disease protection, in complex areas like sub-Saharan Africa?
Resolving the malaria challenges?
Professor of Cell Biology and Infectious Diseases
- An increase in malaria often signals societal issues, poor infrastructure or the failure of a country’s health system. The challenges of the infectious disease are the challenges of society, sometimes as basic as the challenges of simple infrastructures.
- There are many innovations that could really be game changers for how we treat disease, and how we treat a particular disease of poverty like malaria. One of them is smart diagnostics, i.e. how diseases are stratified, how they are placed on the map.
- Smart diagnostics, smart mapping and smart understanding of the distribution of disease is important for breaking some of these key cycles. We combine that with the “Swiss Army knife” approach to global infectious diseases.
- The most powerful thing you can do is empower local community, nurses and healthcare workers to understand, diagnose and treat disease. Local empowerment mixed with local capacity-building is a real innovation.
- We need to invest much more in malaria research and the translation of research to make a difference to communities. If you release the economic stranglehold that malaria puts on communities, the change will be phenomenal.
The canary in the mine
Resolving the challenges of public global health, especially for Africa, is a hard challenge. It is a jigsaw puzzle of different problems that make it difficult to address the malaria disease – which I work on – or any of the other diseases that plague low- and middle-income countries around the world.
One of the things that strikes me about malaria is that it is the canary in the mine. It is the first signal that a country’s health system or infrastructure is falling apart. Interestingly, in Venezuela, which recently underwent a political collapse, one of the first diseases that started to bounce back and appear was malaria. The same thing has happened in countries in Africa, where children, in particular, face many different challenges. Often when a country is not doing well, the rate of malaria will skyrocket.
Infrastructure, poverty and malaria (or how far is the nearest bus stop?)
Now, we are living in a time with a global pandemic of a new virus. One of the dangers is that our response to a new disease is to lose focus of the ongoing challenges of something like malaria. Anecdotally, people have talked about the Ebola outbreak that happened last year and over the last several years in Africa, in Western Africa in particular. But, actually, a lot of people who died at that time died from malaria. This was well understood. They were dying because the local health system collapsed. More people stopped going to clinics. If you had a fever, would they assume you had Ebola and not want to go near you?
As somebody who has worked on malaria and has started to look beyond the lab to the field and global health in general, you realise that the challenges of the infectious disease are the challenges of society. Sometimes they are as basic as the challenges of simple infrastructure. Professor Brian Greenwood from the London School of Hygiene and Tropical Medicine quotes this statistic, which always stuck with me as a student: one of the greatest indicators you have of dying from a disease like malaria is how close you live to a bus stop. That was a lightbulb moment for me. A lot of these challenges in the developing world are challenges of infrastructure, economics and poverty.

Place a disease on a map
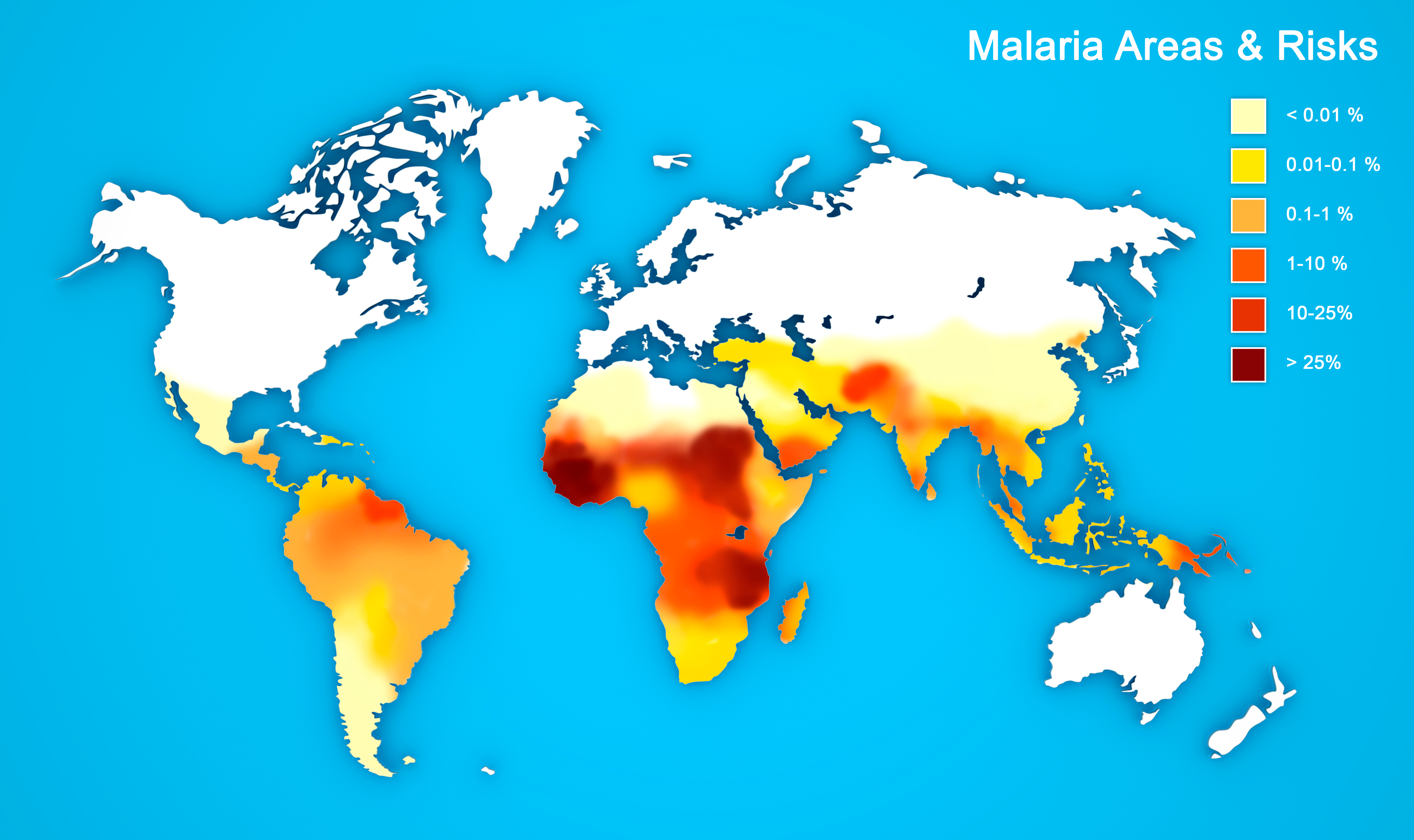
There are many innovations that could really be game changers for how we treat disease, and how we treat a particular disease of poverty like malaria. One of them is smart diagnostics. The global community is becoming aware that it is not enough to just diagnose a disease – malaria, tuberculosis, Ebola or any other infection – but you need to place it on the map.
If you understand how diseases are stratified, how they are placed within different areas, then you can start to tailor your interventions geographically. Maybe the map is heterogeneous; maybe you know there is a village that has intense transmission of a disease, and there is another village that has much less but still has a constant reservoir of disease. If you understand that, then you can tailor where your interventions are going to be.
Why smart diagnostics are needed
In a community with very high transmission of malaria, you need to be able to take care of sick children, treat them quickly and disseminate curative drugs. In other areas, where there is very little disease from malaria, but there is a lot of asymptomatic malaria, you might need an entirely different strategy. So, rather than taking a blanket approach of giving everybody in Africa a bed net or a pill, for example, it may be that certain areas would benefit from strategies that reduce local mosquito populations or reduce transmission disease. In other areas, the strategy might be getting rid of that infectious reservoir to break the cycle of malaria.
Another disease which we might not be conscious of, but which is still important for a different reason, is polio. Polio was rampant across the world in the 1950s and before. Then there was a vaccine. And now we are on the cusp of polio eradication. But the last steps of polio eradication have been hard to achieve. Why is that? Part of it is because we have taken this blanket approach. It is like the “whack-a-mole” game. You try to eradicate it in one area; you try to eradicate it in another area. It just keeps popping up, and you cannot control it. So, you need spatial awareness. You need to understand the entire lay of the land. Often, you will find villages that are not on maps. There are areas that are not connected to public health infrastructure, where you have a disease reservoir.
Taking a “Swiss Army knife” approach
Smart diagnostics, smart mapping and smart understanding of the distribution of disease is important for breaking some of these key cycles. We combine that with the “Swiss Army knife” approach to global infectious diseases. You need strategies to cure, so you need drugs; you need strategies to prevent, so you need vaccines; and in the case of malaria, you need to be able to control the vectors, so you need vector control. Whether that is spraying insecticides within houses, or even genetically modified strategies to get rid of the mosquito, you need public health infrastructure, awareness, consultation and diagnostics. You need this plethora of approaches to deal with a disease.
Ironically, malaria is actually a treatable disease, like many other diseases. That points to our need for strategies that will help us to identify where an intervention is best placed, and where we need to go in order to bring a disease under control. For a continent as mixed and as fascinating as Africa, with so much variation in wealth and infrastructure, we need this nuanced “Swiss Army knife” approach to diseases to make a seismic change in global health. We need awareness: an eye-opening understanding of the lay of the land and how the disease is stratified.
How GPS enhances smart diagnostics
For a spatial understanding of how stratified areas like sub-Saharan Africa might be for global health, two innovations are really important. The first is this incredible access to GPS, this idea that we can know where we are globally. In many developing areas of the world, there is a lack of infrastructure for telecommunications. But now with mobile phone technology, you can know where you are. With the geographical knowledge of GPS systems and mobile phone technology, you can not only diagnose in the field but you can place that diagnosis in the field.
Traditionally, we diagnose malaria down the microscope, or using a basic tool like a pregnancy test, which says yes or no. There are false negatives with those. They also do not give us much nuanced information. But new smart diagnostics, which are based on either DNA or complex protein signatures, can tell you about somebody you didn’t even know was infected, or who is infected with a particular species or particular strain of disease. We can place that using GPS technology in a way that we never could before. So that is the first innovation that I would point to. That is a game changer.
A shift in cultural awareness
But perhaps even more important is an innovation of cultural awareness. For a long time, our approach to the disease of the developing world, in particular, has been dominated, especially in the West, by this idea that we go to. As a white British scientist, I go to Africa, impart my knowledge and try to effect change. Now, there is a seismic shift in that.
This change is terrific to see. It is empowering African scientists and the African community to own their own disease, control infrastructure and engage with communities. Whether it is the regional or even the foreign worker who is coming in to diagnose, it is local community, nurses and healthcare workers who are empowered with understanding how to make a diagnosis of disease, how to treat that disease. Sometimes the most powerful thing you can do is empower that local knowledge base to understand, diagnose and treat disease.

Innovations in hardware and software
Some people today talk about hardware and software, and the need for innovations in both. I like that analogy because hardware relates to innovations such as GPS technology for diagnostics and state-of-the-art digital satellites. I can say where and when somebody is infected. But the software is just as important, and the software is the people power. It is the interaction between the empowered local healthcare worker or the science community, whether that is in the West or in Africa. There is a booming African science industry, which is terrific to see. There are African discovery drugs being made in Africa for African diseases.
Local empowerment mixed with local capacity-building at the level of healthcare workers and healthcare systems, at the smaller scale, is a real innovation. That will change the way that some of these important diseases in the developing world are eventually conquered. They will be conquered locally rather than by this colonialist mentality of going somewhere and getting rid of a disease. Those two innovations stand out in the hardware and software of global health technology.
Bringing malaria to its knees
We have all witnessed a new disease come about. In two weeks or so, scientists had sequenced the genome of the COVID-19 virus. The speed at which science has progressed, the amount of money thrown at developing a vaccine, is incredible. It is amazing when the science community comes together, and when all the resources you need are provided.
Hundreds of millions of doses of COVID-19 vaccines have been ordered and given to people, in one year, for one new disease. As a malaria researcher, you think: we have had malaria for 50 years. We have had so many eradication plans, and yet we are still not there. It is a different disease. It is not a virus. It is more complicated than the COVID-19 virus. So, it is going to be a challenge to bring malaria to its knees. But it is treatable, and it is curable if the infrastructure is there.
The reason why malaria has not shifted is that it needs a huge amount of attention and investment. But it is worth it. The irony is that, as a global community, we are stressing out about the number of people who are dying from COVID-19. But half a million children die each year from malaria. And that is doing the best we have ever done, certainly in the last 20 years.
What if profit did not matter?
At the turn of the millennium, a million children were dying from malaria each year. With mobilisation of the appropriate resources, if we could throw the same proportional weight at malaria, advances in vaccinology could be made. Currently, it is not profitable to make a vaccine for malaria, but it is profitable to make a vaccine for the COVID-19 that is infecting the Western world. What if profit was not an issue? If those resources went into making a malaria vaccine, we would be a lot further ahead. The same is true for drugs and all the other strategies.
We need to invest much more in malaria research and the translation of research to make a difference to communities. It is worth it, not only because hundreds of millions of people are infected with malaria each year, and around half a million die, but also, if you release the economic stranglehold that malaria puts on communities, the change will be phenomenal. If we invested in malaria the way we have invested in other diseases, it would make a huge difference.
We live in an incredible time where the technology is available. The speed of research is breathtaking. If we can apply that as a sharing, generous community, eradication of malaria is within our grasp. Maybe not in our immediate lifetime, but we can move towards it within the next 25 or so years – so, why not? It is doable and with the right motivation, we could do it.
Discover more about
progress towards malaria eradication
Zubiaurre, A., Yahiya, S., Fischer, O. et al. (2020). Structure–Activity Relationship Studies of a Novel Class of Transmission Blocking Antimalarials Targeting Male Gametes. Journal of Medicinal Chemistry, 63(5), 2240–2262.
Delves, M. J., Miguel-Blanco C., Matthews, H. et al. (2018), A high throughput screen for next-generation leads targeting malaria parasite transmission. Nat Commun, 9(3805).